Association of grandmaternal and maternal age difference at delivery with maternal pregnancy cardiometabolic disorders
Published 09 July, 2025
In a retrospective cross-sectional study based on the "Grandmothers, Mothers, and Their Children’s Health (GMATCH)" cohort in Huai’an, China, researchers analyzed data from 2,235 grandmother-mother pairs to explore whether a larger age difference between grandmothers and mothers at delivery is associated with an increased risk of maternal pregnancy cardiometabolic disorders (CMDs). The age difference was defined as grandmaternal age at delivery (grandmother’s age at the time of the mother’s birth) minus maternal age at delivery (mother’s age at the time of the child’s birth).
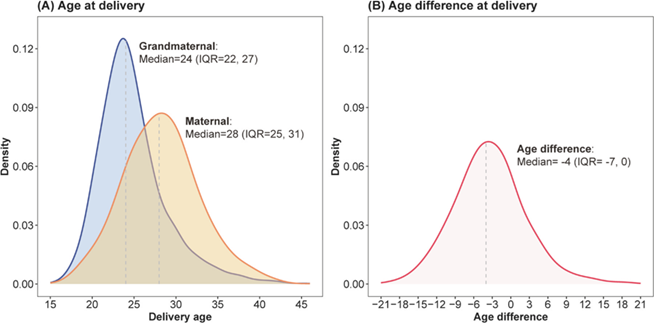
Notably, the researchers found that the median delivery age increased from 24 years in grandmothers to 28 years in mothers, with age differences ranging from -21 to 21 years. A delivery age difference of ≤-9 years was significantly associated with an elevated risk of pregnancy CMDs.
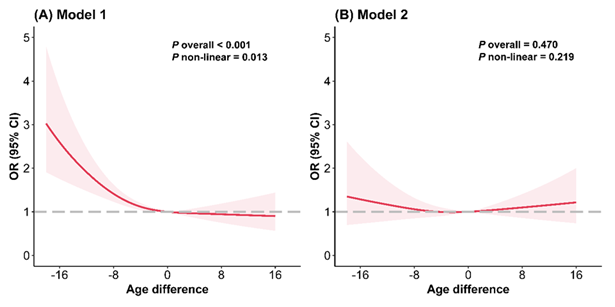
"Dose-response analysis showed a nonlinear L-shaped association: as the age difference increased from 0 to -21 years, the risk of CMDs increased, while it stabilized when the difference was positive," explains senior author of the study, Prof. Xiaolin Xu, from Zhejiang University School of Medicine. "Although the association weakened after adjusting for maternal age, our study underscores that intergenerational age dynamics may reflect underlying biological or lifestyle changes that influence pregnancy health."
The global trend of delayed childbearing has raised concerns about maternal CMDs, but prior research has focused primarily on maternal age alone.
“This study is among the first to examine how grandmaternal delivery age contributes to these risks, says Xu. “Healthcare providers should consider both maternal and grandmaternal age when evaluating CMD risk factors.”
Contact author: Xiaolin Xu, School of Public Health, The Second Affiliated Hospital, Zhejiang University School of Medicine, Hangzhou, Zhejiang, China, xiaolin.xu@zju.edu.cn
Funder: This study was supported by grants to XX from the China Medical Board Open Competition Program (21−416) and XZ from the Jiangsu Maternal and Child Health Program (F201932).
Conflict of interest: Xiaolin Xu is an editorial board member of Healthcare and Rehabilitation but has not been involved in the journal’s review or decisions related to this manuscript. The authors declare no conflicts of interest.
See the article: Cheng Y, Ding W, Zhang Y, Wang H, Zhu X, Xu X. Grandmaternal and maternal age difference at delivery with maternal pregnancy cardiometabolic disorders: a cross-sectional study from grandmothers, mothers, and their children’s health study. Healthc Rehabil. 2025;1(2):100020. doi:10.1016/j.hcr.2025.100020.